|
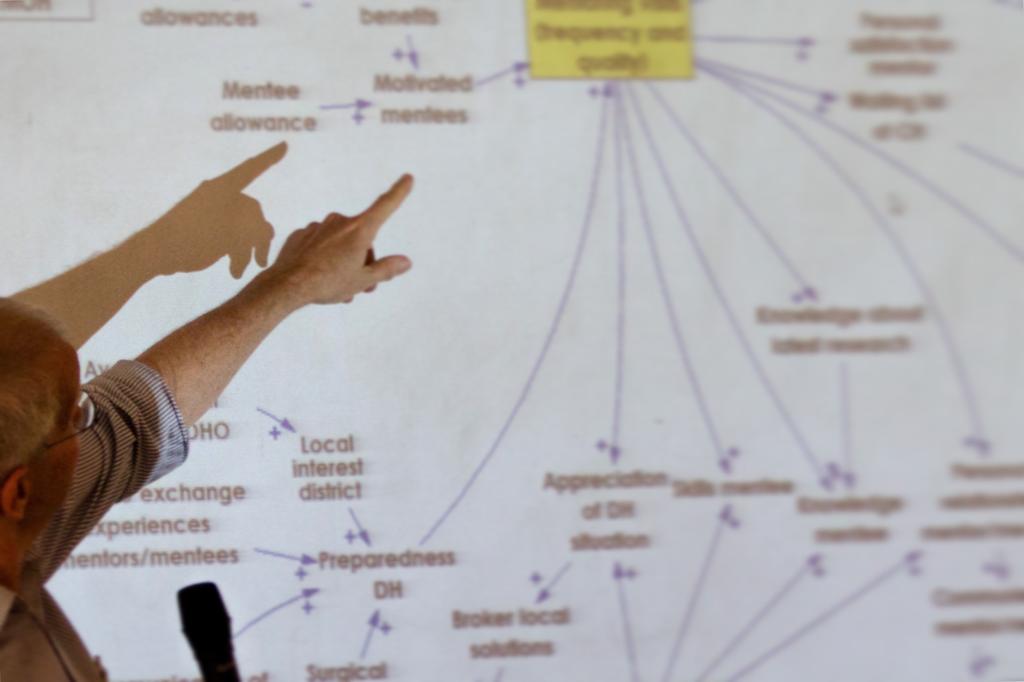
Based at Radboud University Medical Centre in Nijmegen, the Netherlands, I have carried responsibility for the health economics arm of SURG-Africa, and of its predecessor COST-Africa. A large chunk of our research was dedicated to establishing the cost of providing and scaling up district-level surgery in Malawi, Zambia and Tanzania. In our studies we looked at the financial costs of all types of resources used in providing surgery, irrespective of whether or not patients pay a fee. Examples of resources included are: staff salaries and other emoluments of surgery providers; medicines, surgical and non-surgical supplies used in theatre or in the ward for post-operative care; surgical patient transport by ambulance; depreciation of infrastructure such as buildings and equipment; maintenance of medical and non-medical equipment used in surgery; utilities (electricity, water, telephone communication); administration and other overhead. We also considered the economic costs (i.e., including depreciation and opportunity costs). This allowed a full costing of the provision of surgery, from the very first clinic consultation to the last follow-up visit. It proved an eye-opener for many of the hospital staff that we worked with: surgery turned out to be much more resource intensive and costly than they had thought. More recently we calculated the cost of surgical referrals by ambulance in the three countries and conducted an analysis of the strategies that district hospitals employ to cope with the high financial burden involved. We found that hospital management teams have already taken various measures to contain the cost of running their ambulances, for instance by transporting two or more patients in a single ambulance trip. And although in some places there may be still some room for efficiency gains, the manoeuvring space for the hospital management teams is limited, which further undermines the fragile financial positions of the hospitals. It is also worth mentioning that several years back (under COST-Africa) we conducted a study in Malawi to establish the direct and indirect costs that patients and their families incur to access essential surgery. Unsurprisingly, we found that out-of-pocket household expenditure was high and in many instances catastrophic, putting households, especially those who are already poor, at risk of further impoverishment. This underlined that scaling-up surgical services in rural areas needs to be accompanied by health insurance or some other form of financial risk protection. As part of our more recent research work we conducted a series of group model building workshops in each of the three countries. The purpose of the workshops was to examine the complexity of scaling-up district-level surgery (in Tanzania) and of surgical team mentoring in support of such scaling-up (in Malawi and Zambia), which forms the core of the SURG-Africa project. The workshop participants represented various parties that have a role in providing surgical services. Through a participatory approach, and supported by our team from Radboud UMC, they developed causal loop diagrams that describe the complexities and cause-and-effect relationships at hand. This provided the basis for a set of very practical policy options to increase access to surgery for rural populations. We shared our summary findings with the workshop participants for their feedback, after which we developed and submitted three articles to scientific journals. We hope the articles will be accepted and published soon, so they reach a wider audience.
It has been a privilege and a joy to work with professionals ‘on the ground’ – hospital managers, clinicians, theatre staff, pharmacy, radiology and laboratory staff, medical records clerks, procurement officers, financial administrators, social welfare staff, transport officers, drivers – sometimes in quite remote places. We appreciate their dedication to work in circumstances that are often far from easy. I say that on behalf of my colleague Martilord Ifeanyichi and my former colleagues Henk Broekhuizen (under SURG-Africa) and Dennis Cornelissen (under COST-Africa), who each spent considerable time in the field conducting interviews and collecting data, which were not always easy to obtain. We have enjoyed the work, the friendly relations, and the nsima/nshima/ugali with chambo/nyama/kuku and tasty relish/soup! We would like to thank the local research coordinators (Mweene Cheelo, Gerald Mwapasa, Adinan Juma) for their support in organising our field trips and in the data collection itself. We look forward to continued interactions with provincial/regional-level health programme officers and national-level policy makers about options and future strategies to scale-up surgery for rural populations in Malawi, Tanzania and Zambia. To access journal articles published on the topic so far, click here. More on Dr Leon Bijlmakers here.
2 Comments
13/5/2023 06:40:48 am
reat post by Dr. Leon Bijlmakers! The way he demystifies health economics and explains it in a clear and concise manner is truly commendable. It's so helpful to have experts who can break down complex concepts into simpler terms, making it accessible to a wider audience.
Reply
12/10/2023 01:46:34 pm
Professor Leon Bijlmakers' work on health economics, particularly in the context of surgical services in African countries, highlights the often underestimated costs involved in providing healthcare. His research sheds light on the resource-intensive nature of surgery and the financial challenges faced by both hospitals and patients. It underscores the need for comprehensive strategies, including health insurance, to ensure access to essential surgical care without pushing households into further financial hardship.
Reply
Leave a Reply. |



 RSS Feed
RSS Feed