|
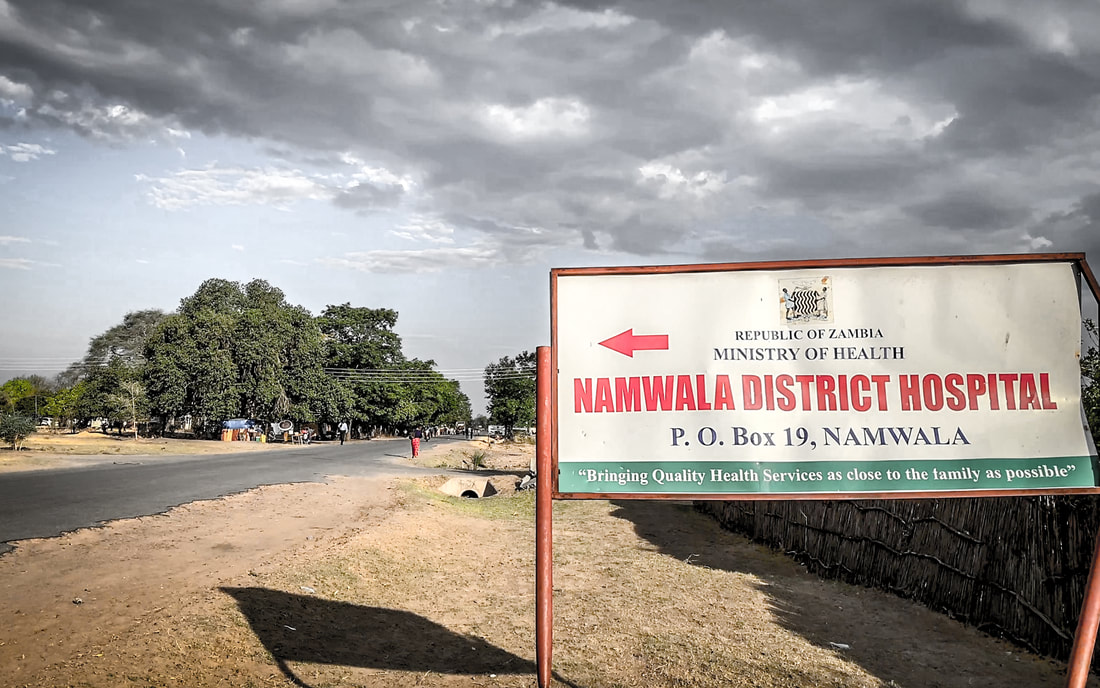
SURG-Africa has been looking at how to scale up access to safe surgery for rural populations in Malawi, Tanzania and Zambia, through strengthening surgical care provided by district hospitals. This has centred on regular in-service training for the surgical teams at district hospitals. Specialists from referral hospitals have visited district hospitals quarterly or bi-monthly for two years to provide mentoring, training and supervision to the local teams. At our initial action-planning workshops, the visiting specialists and district hospital teams worked together to compose site-specific training visit plans for each hospital and agree the priority areas for skills training and mentoring. These were also informed by detailed analyses undertaken by the SURG-Africa teams on the surgical activity at each district hospital and focus group discussions at baseline participatory action research workshops in each country. During this process, we realised there was in most cases a lack of set local or national guidance about the scope of surgical care that district hospitals should provide, i.e. which surgical cases should be done at district-level hospitals, and which should be referred to a higher-level hospital. It is really important to advance understanding on the level of surgical care that district-level hospitals are expected to provide, as this influences how to plan staff training and development, guidance to give on making appropriate referrals to higher-level hospitals, and advocacy for necessary resources, infrastructure and personnel for district hospitals. We had the opportunity to ask regional surgeons and anaesthetists attending a conference of the College of Surgeons of East, Central and Southern Africa (COSECSA) their opinions on this subject in December 2018. We have reported our results in our paper ‘Which Surgical Operations Should be Performed in District Hospitals in East, Central and Southern Africa? Results of a Survey of Regional Clinicians’ It was very interesting to discover that there were clear areas of consensus amongst respondents across 15 countries about the types of operation that should and should not be done at district level, but there was a group of operations including bowel resection and anastomosis where there was quite a mixed response and difference of opinion about where these should be done and who should undertake these cases. As well as considering the opinions of experienced surgical providers in the region, we are interested in what surgery is already happening in district hospitals. Our SURG-Africa colleagues have collected data on the surgical activity of the intervention and control district hospitals in our research sites (published here, and more publications to follow). While this is really useful data on district hospitals in Malawi, Tanzania and Zambia, we are also interested in what surgery is currently done in district hospitals across Africa. We wanted to get a general overview of the reported current surgical capacity and delivery to help us understand district hospital surgical activity better and suggest targets for further development and research in the region. We undertook a scoping review on surgery in district hospitals to find out, according to published literature:
We searched PubMed and Ovid EMBASE for publications from January 2000 to December 2019. We included studies if they contained information about types of surgical procedures performed, number of operations per year, types of anaesthesia delivered, cadres of surgical/anaesthesia providers and/or patients' outcomes. Our results showed what we suspected, that there was a paucity of published data about what was happening in district hospitals. This is perhaps not surprising as most district level hospitals would be unlikely to submit articles to peer reviewed journals. However we did find 52 relevant publications which provided information about 16 countries. These demonstrated that district hospitals were a group of diverse institutions ranging from 21 to 371 beds. The three most frequently reported procedures were caesarean section, laparotomy and hernia repair, but a wide range of orthopaedics, plastic surgery and neurosurgery procedures were also mentioned. The number of operations performed per year per district hospital ranged from 239 to 5233. The most mentioned anaesthesia providers were non-physician clinicians trained in anaesthesia. They deliver mainly general and spinal anaesthesia. Depending on countries, articles referred to different surgical care providers: specialist surgeons, medical officers and non-physician clinicians. 15 articles reported perioperative complications among which surgical site infection was the most frequent. Fifteen articles reported perioperative deaths of which the leading causes were sepsis, haemorrhage and anaesthesia complications. We concluded that district hospitals play a significant role in sub-Saharan Africa, providing both emergency and elective surgeries. Most procedures are done under general or spinal anaesthesia, often administered by non-physician clinicians. Depending on countries, surgical care may be provided by medical officers, specialist surgeons and/or non-physician clinicians. Research on safety, quality and volume of surgical and anaesthesia care in this setting is scarce, and more attention to these questions is required. Our full findings are published here in ‘Surgical care in district hospitals in sub-Saharan Africa: a scoping review’. Professor Chris Lavy and Grace Drury, NDORMS, University of Oxford.
3 Comments
30/3/2023 03:45:51 am
Respectfully Sir,s/Mam
Reply
29/12/2023 11:33:07 am
Acknowledging Prof. Chris Lavy and Grace Drury's blog on Surg Africa, I commend their valuable insights into surgery in Sub-Saharan Africa.
Reply
Leave a Reply. |



 RSS Feed
RSS Feed